What "value-based care" means and why it is good for physical and financial health
September 16, 2020Last month, Blue Cross and Blue Shield of Minnesota announced a significant value-based agreement with Allina Health, the largest health care provider system in Minnesota. You may have seen or heard this news and wondered why this type of agreement matters to you, the patient.
For more than a decade, value-based care has been discussed as a potential solution to many of the challenges the U.S. health care system faces, including rising costs and worse health outcomes across the country.
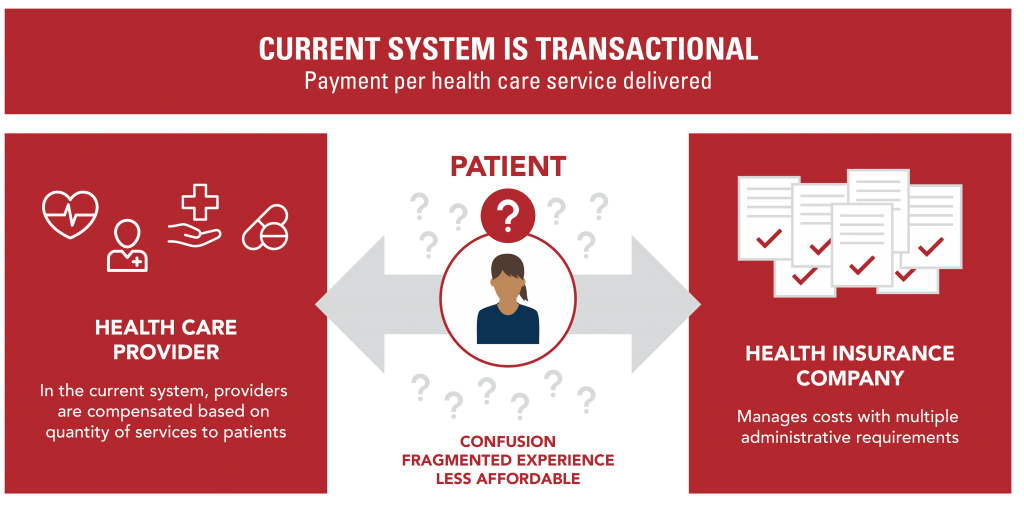
The idea is simple: instead of paying for health care based solely on the number and types of services provided to a patient (tests, scans, surgeries, office visits, hospital stays, etc.), health care should be paid for based on the outcomes of those services and the overall health of the patients that receive them.
Here are three key ways this is done through a value-based care model:
- Encourage focus on preventive care to keep people healthy, rather than care that is given in response to sickness.
- Ensure the focus is on patients receiving the right care at the right time and right place.
- Reduce unnecessary care, which ultimately leads to higher health care prices without improving health.
A simple idea, a complex reality
Sounds easy enough, but making a value-based care agreement a reality is complex. In fact, there are only a handful of examples of these types of agreements that go far enough to make a significant difference on health and health care costs. This is because in order to be effective, value-based care agreements require significant trust and collaboration between health plans and health care providers.
They also require a very strong effort by both parties to move away from the traditional methods of paying for care. Instead, insurers and health care systems must work collaboratively to create a completely new way of doing business. And, finally, the organizations must work together to find a way to ensure, first and foremost, that this new model benefits the patient.
As Allina Health’s president and CEO, Dr. Penny Wheeler, recently put it, “We are committed to delivering even better quality and affordability to those served and will put in the hard work required of this agreement to do just that.”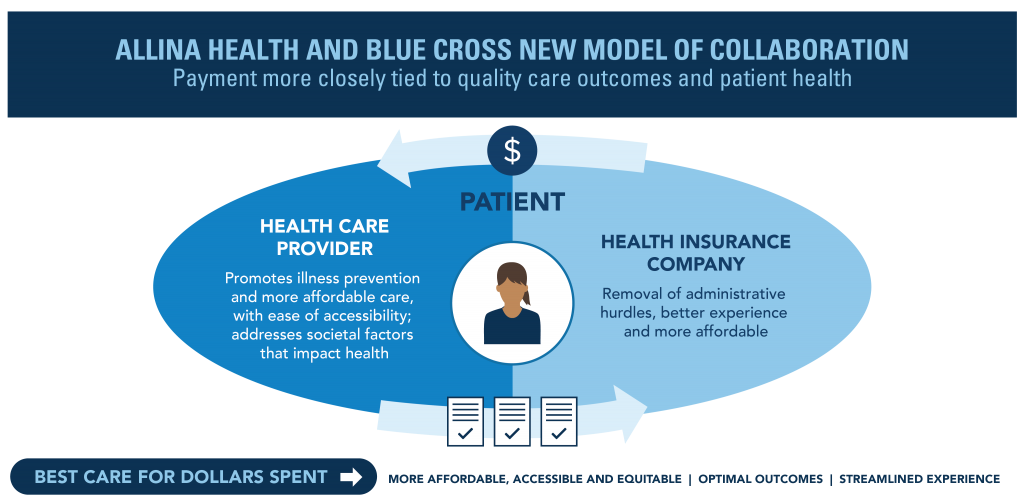
Why the change is needed now
For far too long, health care in the U.S has been paid for based on the volume of care instead of the value of care provided.
What this means is that, over time, the focus has become less on the patient’s health outcomes and more on the number of tests and procedures done. Blue Cross believes that this traditional “fee-for-service” payment model is outdated and the foundational change necessary to create a lasting impact on our members' physical and financial health is long overdue.
In recent years, we have come to the table with health care providers to discuss the possibilities of making this foundational change a reality. Providers including Allina Health, Minnesota Oncology, Mayo Clinic, North Memorial, and, most recently, the 47 independent primary care clinics that make up the Minnesota Healthcare Network have all worked with Blue Cross to launch innovative value-based care agreements.
Pandemic proves need for value-based care
The health crisis brought on by the COVID-19 pandemic shows why value-based care is an effective way to improve the long-term sustainability of the entire health care ecosystem in Minnesota and beyond. In response to the pandemic, many services, such as elective surgeries, were delayed or limited, causing great financial strain for health care systems throughout the country.
Alternatively, in a value-based care model, providers receive a more stable income stream based on quality of outcomes, not quantity of services, ensuring they are better able to weather the ups and downs like those seen throughout the pandemic.
How this changes the member experience
As the shift to value-based care continues to build momentum, members may notice their doctor or nurse has more time to discuss other elements of health, including social determinants (health outcomes based on where you live, work and play). The goal is for health care providers to have more time to focus on more proactive forms of preventive care with less administrative burden. This means more time spent building patient relationships, streamlining the care delivery experience and reducing burnout.
You may also notice additional options available for care outside of the traditional hospital or clinic setting. Virtual and in-home care, which often cost less and can be just as effective, may become more common. These alternatives also aim to remove barriers to receiving care, such as travel to and from an appointment, creating a more equitable health care system.
The end goal
Ultimately, value-based agreements aim to help more Minnesotans become and remain healthy for the long-term, while also slowing the dramatic increase in health care costs seen in recent years. Blue Cross will continue working closely with health care providers across the state to create a sustainable health care ecosystem for our members.
Read more
An important part of value-based agreements is making sure health plans and providers are gathering, tracking and using the appropriate data to determine where improvements are needed and how well the program is working. Read more about how this is done in this previous blog post.