Spot the signs: five things to remember during Mental Health Awareness Month
May 16, 2024
This article is written by guest contributor Dr. Brett Hart, vice president of behavioral health and mental health parity at Blue Cross and Blue Shield of Minnesota.
One of my favorite films is the 1999 classic psychological thriller The Sixth Sense. Without giving away the infamous “twist ending,” the movie expertly shows how perception and reality are not always one in the same. Oftentimes, things can look different, depending on perspective.
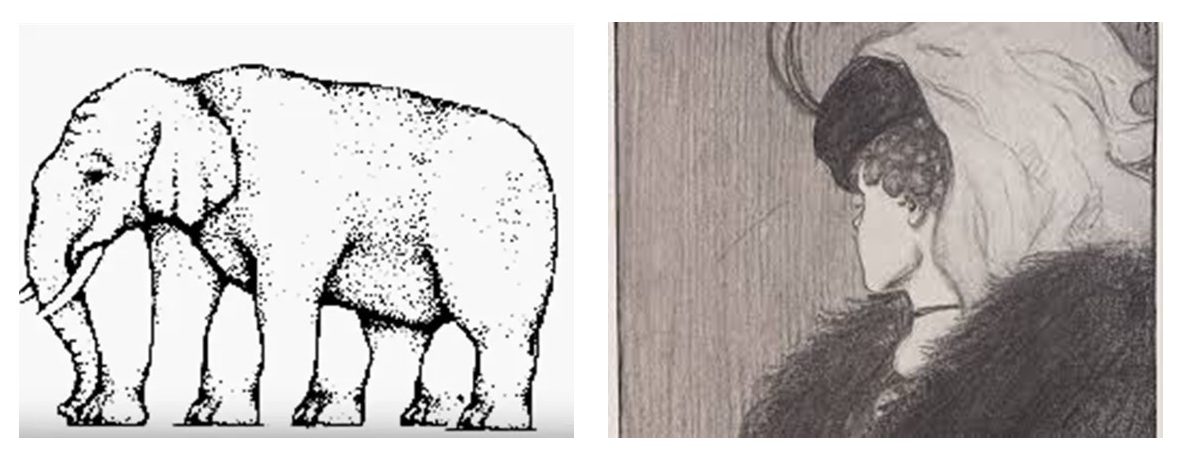
For example, look at the pictures below. In the left, how many legs does the elephant have? In the right, do you see an aging woman looking down or a young woman looking away?
While suspenseful movies and optical illusions can be harmless tricks of the mind, real life perceptions – especially involving our behavioral and physical health – can impact health decisions and, ultimately, outcomes.
Sometimes, symptoms of a behavioral health condition can present as a physical issue. In other circumstances, physical ailments may present as a behavioral health issue. How we make sense of our physical and emotional experiences can directly correlate to how, or even if, we choose to address them.
Two of the most common behavioral health conditions are depression and anxiety. As many as one in five people experience moderate levels of depression, while one in four experience moderate levels of anxiety. Common symptoms of these conditions include digestive issues, headache, fatigue, and sleep disturbance. For many, the presence of such symptoms would lead them to see their primary care physician or a specialist. In fact, 80 percent of patients with a behavioral health condition will first visit their primary care doctor. Often, this is due to individuals focusing on the physical nature of their symptoms, coupled with a feeling of stigma about behavioral health conditions leading to a hesitancy to view symptoms as being tied to a behavioral health condition.
This phenomenon can also be seen in reverse. An individual may experience behavioral health symptoms and assume they have a behavioral health condition when, in fact, the symptoms are the result of a physical condition. One example is an individual who feels nervous and jittery with an increased heart rate, thinking this may be the result of anxiety, when it is due to high blood pressure. Not only can symptoms be mistakenly attributed to behavioral health or physical health conditions, but behavioral health and physical health conditions can cause one another. For example, chronic anxiety can cause gastrointestinal conditions, while chronic pain can lead to depression.
Disentangling what symptoms are attributable to what conditions, or sorting out what is cause and what is effect is not only confusing for a patient, but can also be confusing for a practitioner. So where does this leave us?
Do we just do our best and guess what is happening? Do we hope our doctor can figure it out?
Fortunately, the process does not have to be a matter of guesswork. There are concrete things we can do to ensure an accurate understanding of our own experiences and those of the people we care about.
1. Be aware of how stigma can influence your thinking
Often, the stigma that still surrounds behavioral health conditions keeps us from even considering that is what we may be experiencing. Challenge yourself to at least consider a behavioral health condition as something that should be ruled in or out once further information is collected.
2. Invite input from others
We all have “blind spots” when it comes to being objective about our health. For this reason, it can be helpful to ask a trusted friend or family member about what they observe in your behavior. Have they seen any mood changes, withdrawal, increased sensitivity, or changes in school or work performance? We don’t want to put the pressure of accurately diagnosing us on a friend or family member, but obtaining feedback from a trusted individual can provide honest and additional data that can be useful.
3. Keep a diary
We live in a fast-paced, in-the-moment world that doesn’t always allow opportunities for self-reflection. For this reason, it can be helpful to keep a “health diary.” On one side of the page, log your activities throughout the day (what you are eating or drinking, who you are interacting with, where you are, etc.) Next to each entry, write down how and what you are feeling and where in your body you feel it. Often, after several days of this activity, we start to see trends emerge such as, “Every time I drive during rush hour, I get pain in my stomach,” or, “Each time I eat something made with flour, I feel nauseous.”
4. Research family history
While symptoms don’t always ‘run in the family’, at times there is a genetic component to both behavioral health and physical health conditions. Part of understanding your own health history is understanding your family health history. Gather data from family members about behavioral health or physical health conditions that blood relatives may have experienced or are still experiencing. Keep a record of these conditions that you can share with healthcare providers.
5. Speak candidly and openly to a professional
Whether speaking to a behavioral health or physical health professional, what we get out of the experience is often related to what we put into it. Talk openly and candidly about your symptoms. Describe them in detail. Explain when they occur and when they don’t. Identify any triggers that bring on or worsen your symptoms. Share your family history. Talk about changes that may be causing stress in your life. Your provider may ask questions that aren’t always comfortable to answer – but making an accurate diagnosis depends heavily on what you are willing to share.
Behavioral and physical symptoms and conditions are not always what they seem and can be difficult to sort through. Of primary importance, however, is to recognize that you don’t have to figure this out alone. By resolving to act, engaging those close to you, and confiding in a trusted professional through open, honest dialogue, there is help available and a path forward.
Check behavioral health benefit eligibility online at www.bluecrossmn.com, within Blue Care Advisor, or by calling the phone number on the back of your member ID card.




Great article, good read and good advice.
Appreciate the article beign front page for our associates in this important month of awareness building – thanks!
Great article!!, Thanks for sharing this critical information.