Take 5: Blue Care Advisor takes the guesswork out of managing your benefits
January 10, 2023Take 5 is a series in which we pose five questions to a Blue Cross associate and learn more about who they are, what they do, and how they help our members live their healthiest lives.

In this edition of “Take 5”, we talk with Matt Hunt, our vice president of customer experience, about Blue Care Advisor, a new technology solution for optimizing health and wellbeing.
What exactly is Blue Care Advisor? Is it a new app? What makes it different?
Wait, isn’t that three questions? (laughs) Simply put, Blue Care Advisor is a new, easy-to-use tool for members to access their health plan. You can choose to use the mobile app or member portal and access all of your benefits in one spot, bring up your insurance card digitally, know the cost of care before getting treatment, receive provider recommendations and earn rewards for healthy behaviors
We have a terrific team that spent the past year developing, building and refining every last detail. Now, it’s brand new for 2023 and will replace our current app and portal. With Blue Care Advisor, members have a “digital front door” for a personalized experience.
When members understand benefits and use them, we are better able to help ensure they receive the right care at the right time, which is both good for their health and their wallet.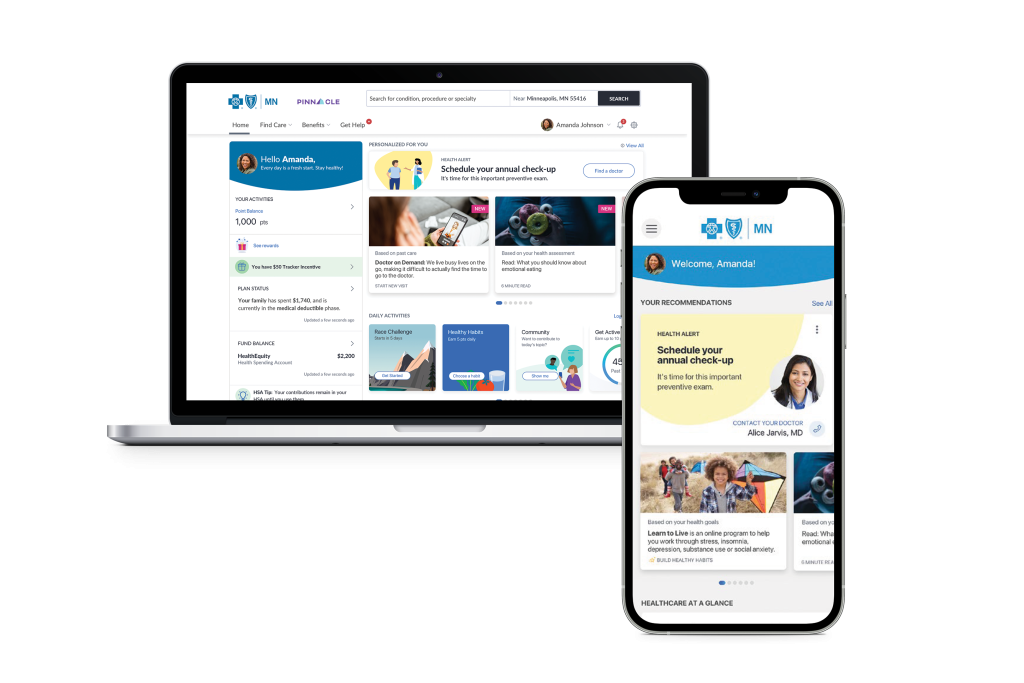
Was there member feedback that prompted you to create Blue Care Advisor?
Members continually tell us that managing healthcare is confusing. People truly want to improve their health, but they’re not always sure how to follow through. Blue Care Advisor was built to help by first asking each member what is most important to them. We then use those answers to offer specific health benefit programs, which come with real support from advocates on our service team.
Can you give a real example of how using Blue Care Advisor can lead to better experiences with Blue Cross?
Let’s say my doctor tells me I’m at risk for developing type 2 diabetes. With Blue Care Advisor, I’m able to select this as an issue I want to address. The app will then let me know that I have access to a free online diabetes prevention program, complete with education, remote monitoring, and healthy behavior encouragement. Then, let’s say life gets busy and I fall behind a bit. The next time I call Blue Cross for any reason, the service associate will be able to see where I’m at in my diabetes prevention program and help me get back on track. The goal of Blue Care Advisor is to leverage the right types of tools and information as ways to help our members live their healthiest lives.
When will members be able to begin using Blue Care Advisor and how will they be informed about it?
We are beginning a phased rollout of Blue Care Advisor to our Commercial Market members (those who get coverage from an employer) throughout the year, with new groups being added every month. Members will be notified that they have access via their employer or Blue Cross directly. By the end of 2023, more than more than one million Commercial Market members will have access to Blue Care Advisor.
What comes next? Is it too early to be talking about Blue Care Advisor 2.0?
The work will continue to move forward. We will always be making improvements and enhancements to Blue Care Advisor and member feedback will be key. Later this year, we’re planning to launch a two-way secure chat function, allowing real-time conversations with service associates or Blue Cross clinicians.
Next up, we are working to make Blue Care Advisor accessible to those members with one of our Medicare plans. We’re really proud of what we’re able to deliver through Blue Care Advisor and can’t wait for members to begin engaging with it.

Eligible Blue Cross Members: Once you have received notification of access, you can begin using Blue Care Advisor via our app or web portal to check in on your benefits, deductible, programs, and more. The Blue Care Advisor app is available in both the Apple App Store and Google Play Store.

